A study to evaluate the effectiveness of Diaphragmatic Breathing and Pursed Lip Breathing Exercise in patients with stable chronic Obstructive pulmonary Disease : Dr.Thatithoti Sudhakar., M.P.T.,; 1 RPR College of Physiotherapy, Ongole, Andhra Pradesh, India; Dr.Kurapati Madhava Reddy, Ph.D., D.Sc., Professor & Principal, Sri Lakshmi Institute of Medical Sciences College of Physiotherapy, Kavali, Andhra Pradesh, India.2
Background: Chronic obstructive pulmonary disease (COPD) has been defined as a disease characterized by air flow limitation that is not fully reversible. The airflow limitation is usually both progressive and associated with an abnormal inflammatory response of the lungs to noxious particles or gases.1
The chronic airflow limitation characteristic of chronic obstructive pulmonary disease is caused by a mixture of small airway disease and parenchymal destruction, the relative contribution of which varies from person to person. Chronic inflammation causes remodeling and narrowing of the small airways. Destruction of the lung parenchyma, also by inflammatory process, leads to the loss of alveolar attachments to the small airways and decreases lung elastic recoil, in turn these changes diminish the ability of the airways to remain open during expiration. Air flow limitation is measured by spirometry, as this is most widely available, reproducible test of lung function.2
Chronic obstructive pulmonary disease is a global health concern and is a major cause of chronic morbidity and mortality worldwide. Many people suffer from this disease for years and die prematurely from it or its complications. The global burden of Chronic obstructive pulmonary disease is projected to be the fifth leading cause of death and Global initiative for chronic obstructive pulmonary disease (GOLD) estimates and suggests that the Chronic obstructive pulmonary disease will rise from the sixth to third most common cause of the death world wide by 2020. The burden of chronic obstructive pulmonary disease in Asia is currently greater than that in developed Western countries.3 Certain occupational exposures like dusts and chemicals and indoor and outdoor air pollutions are also associated with increased risk of chronic obstructive pulmonary disease.
Global initiative for chronic obstructive pulmonary disease (GOLD) aims to improve prevention and management of Chronic obstructive pulmonary disease through a concerted world-wide effort of people involved in all facets of healthcare and health care policy, and to encourage an expanded level of research interest in this highly prevalent disease.4
This conceptual frame work also emphasizes that chronic obstructive pulmonary disease is usually progressive if exposure to the noxious agent is continued. The staging is based on airflow limitation as measured by spirometry which is essential for diagnosis and provides a useful description of severity of pathological changes in chronic obstructive pulmonary disease. The overall approach to managing stable
1
chronic obstructive pulmonary disease should be characterized by a stepwise increase in treatment, depending on the severity of the disease. The classification of severity of stable chronic obstructive pulmonary disease incorporates an individualized assessment of disease severity and therapeutic response in to the management strategy.5
The goal of pulmonary rehabilitation program is to reduce symptoms, improve activity and daily function, and restore the highest level of independent function in patient with respiratory disease. Diaphragmatic breathing is an exercise to better use and to strengthen the diaphragm, the major and most efficient muscle of breathing. Regular practice of diaphragmatic breathing can help restore function of diaphragm and return to a more efficient breathing pattern. Practicing a deeper diaphragmatic style of breathing can help ease of work of breathing and expect more stale air.6
Pursed lip breathing is performed as expiratory blowing against pursed lips, is a pulmonary rehabilitation strategy instinctively or voluntarily employed in patients with chronic obstructive pulmonary disease to relieve or control dyspnea. Six-minute Walk test is simple, easy reproducible and requires no apparatus. It is a self-paced exercise that patients could perform this test alone. It can be carried out at same time of the day at any time.
Reduction of maximum expiratory rate, slow forced emptying of lung and breathlessness are common problems seen in chronic obstructive pulmonary disease. In severe cases of chronic obstructive pulmonary disease, the use of accessory muscles was increased. Diaphragmatic breathing exercise and Pursed Lip Breathing are effective to relieve the symptoms. In other studies, functional performance of the chronic obstructive pulmonary disease patients is not evaluated. Hence the study was undertaken to evaluate the effectiveness of Diaphragmatic Breathing and Pursed Lip Breathing Exercise in patients with stable chronic obstructive pulmonary disease along with the flow rates and rate of perceived exertion.
Aims & Objectives: The aim and objective of the study is to evaluate the effectiveness of Diaphragmatic Breathing and Pursed Lip Breathing Exercise in patients with stable chronic obstructive pulmonary disease.
Method: The chief objective of this study was to compare the effectiveness of Diaphragmatic Breathing and Pursed Lip Breathing Exercise in patients with stable chronic obstructive pulmonary disease. The study subjects were divided in two groups Group A and Group B comprising of 15 patients each. Group A received diaphragmatic breathing exercise and Group B received the pursed lip breathing exercise. Both groups were trained twice daily for 15 minutes for 6 days per week for 6 weeks. Pre
and Post test was done by using 6 Minute Walk Test (6MWT) and spirometry for measurement of FEV1 and FVC. Data was analyzed using a paired ‘t’ test to find out within group difference of dependent variable and a univariate analysis of variance to find out between group differences. All data was analyzed using SPSS version 12.0 with significance level kept at 0.05.
Results: Results also showed that subjects in Group A who received diaphragmatic breathing exercise showed significant improvement in 6 MWT than Group B who underwent pursed lip breathing exercise. Subjects in Group B who received pursed lip
2
breathing exercise showed significant improvement in FEV1 and FVC compared with Group A who received diaphragmatic breathing exercise. But there was no significant improvement in FEV1 and FVC in diaphragmatic breathing exercise group from pretest to post test. In both groups there was significant improvement in 6MWT from pretest to post test.
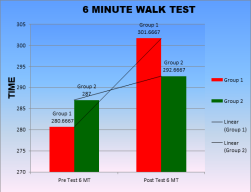
A t-test was done to analyze the within group difference of six-minute walk test which shows that there was a significant improvement for six minute walk test in Group A from pre to post T value (14, 0.05) = -10.088, P<0.000. Group B also showed a significant improvement from pre to post for six-minute walk test. T value (14, 0.05) = -6.859, P<0.000. Univariate analysis of variance was done to analyze the between group difference of six-minute walk test and showed a significant difference between groups, F value (1, 27, 0.05) = 45.645, P<0.000.
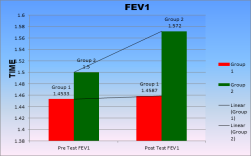
A t-test was done to analyze the within group difference of FEV1 and there was no significant difference for FEV1 in group A from pre to post. T value (14,0.05) = -0.866, P<0.401. But Group B showed a significant difference from pre to post for FEV 1, ‘t’ value (14,0.05) = 6.144, P<0.000. Univariate analysis of variance was done to analyze the between group difference of FEV1 and showed a significant difference between groups, F value (1, 27, 0.05) = 29.25, P<0.000.A t-test was done to analyze the
within group difference of FVC and
there was no significant difference
for FVC in group A from pre to post.
T value (14,0.05) = -1.684, P<0.114.
But Group B showed a significant
difference from pre to post for FVC,
‘t’ value (14,0.05) = –
4.971, P<0.000. Univariate analysis
of variance was done to analyze the
between group difference of FVC
and showed a significant difference between groups, F value (1, 27, 0.05) = 24.681, P<0.000
3
Group B showed a significant difference from pre to post for FEV 1,T value (14, 0.05) = 6.144,P<0.000 and it was supported by Bianchi R et al75 who assessed the volumes of chest wall compartments using a nopto electronic plethysmograph and concluded that by decreasing respiratory frequency and lengthening expiratory time, pursed lip breathing decreases end expiratory volume of chest wall, and also decrease in end expiratory volume of abdomen and modulates the breathlessness.
Thoman R7 proposed that those segments of lungs with greatest fall or greater increase in flow resistance will receive disproportionately less of the tidal volume. Therefore, the abnormal and uneven distribution of gases in emphysema will be accentuated with increased respiratory rate. So, the slowing of respiration alone would be expected to enhance the ventilation of those subdivisions of the lung which normally are under ventilated and found that tidal volume increases while respiratory rate decreases and CO2 elimination improves without significant change in forced residual capacity and volume of slow space by pulsed lip breathing. They found that indeed there was an increase in ventilatory rates of those most slowly ventilated lung components, when respiratory rate slowed down with pursed lip breathing.
Mueller et al8 as well as other investigators found that although pursed lip breathing was more effective in the sense that less air exchange was required to absorb a given amount of oxygen, there was no increase in oxygen uptake This suggests that PLB does not significantly alter the work of breathing. It is known that hyperactivity of the inspiratory muscles is a cause for the sensation of dyspnea. Their assumption that decreases in dyspnea sensation which is often thought to be related to pursed lip breathing might be caused by reduced activity of respiratory muscle is still a matter of debate. Through encouraging the use of diaphragm, the principal and efficient muscle of inspiration, the oxygen cost of breathing can be decreased. Decreasing the use of accessory muscles also decreases the work of breathing. The bio feed can be used to discourage accessory muscle firing during the ventilatory cycles. Because use of the diaphragm as in diaphragmatic breathing was found to increase rather than decrease the level of dyspnea at present routine use of diaphragmatic breathing in pulmonary rehabilitation is not recommended.
Killian9 and coworkers showed that exercise capacity in chronic obstructive pulmonary disease patient is mainly limited by subjective symptoms such as muscle fatigue and dyspnea without the patient reaching their physiological limitations. Now as this is well known that a “vicious cycle” of exertional dyspnea, exercise and activity limitation, psychosocial illness are the major causes of poor health related quality of life in chronic obstructive pulmonary disease. patients there are increasing evidence that physical reconditioning which is most essential component of pulmonary rehabilitation can improve the exercise capacity and health related quality of lives and also found in their study that breathing retraining increases exercise performance in subjects with severe chronic obstructive pulmonary disease.
Schans et al10 observed that positive expiratory pressure breathing which is in range of mouth pressure reached during expiration with pursed lip in patients with chronic obstructive pulmonary disease increases the efficiency of ventilation at rest and during exercise, since same work load is achieved with less ventilation. So, the improvement
4
in exercise tolerance seems to be due to the decrease in the sensation of dyspnea. That’s why these patients do not feel panic at the time of respiratory distress. Their self-confidence could be improved, which progressively increases activities of daily living that mimics exercise of physical reconditioning that can ultimately restore the patient to the highest level of functional capacity and improved health related quality of life. However, the effect on quality of life has not been evaluated by other workers.
Evidence suggests that diaphragmatic breathing does not change regional ventilation in people with chronic obstructive pulmonary disease. This technique increases total ventilation but if so, this suggests this may due to the slower, deeper breathing patterns that may occur during Diaphragmatic Breathing rather than an exaggeration of abdominal motion. Some authors noted an increase in the work of breathing; this may be due to increased paradoxical rib motion during Diaphragmatic Breathing. The relaxed expiration effects of less air tapping, results in reduction of hyperinflation, which turns into reduced respiratory rate, dyspnea and improved tidal volume and oxygen saturation in resting condition. A study by Gosse link 11 proved deep breathing exercise which includes diaphragmatic breathing immediate decrease respiratory rate, dyspnea and anxiety. Jones et al12 confirmed that Diaphragmatic Breathing results lower oxygen cost and respiratory rate.
The study of Levine et al.24 provides the first evidence that appropriate adaptive response occurs in the inspiratory inter costal muscles of patients with chronic obstructive pulmonary disease. Levenson et al13 states that abdominal muscle contraction should be encouraged to lengthen the diaphragm and increase its force generating capacity. Ambrosino et al.14 reported improvement in maximal exercise tolerance in mild chronic obstructive pulmonary disease patients undergoing deep Diaphragmatic breathing. Campbell15 and friend postulated that the increased abdominal motion during Diaphragmatic breathing may shift ventilation towards the base of the lungs. Brach et al 16found that Diaphragmatic breathing did not alter regional ventilation for the group as a whole. Unfortunately; the authors were not able to explain this finding. The study by Sackner et al17 demonstrated that half of the subjects had minimal abdominal displacement during Diaphragmatic breathing. Another study by Sackner et al17 showed that Diaphragmatic breathing was associated with distorted chest wall motion. Diaphragmatic breathing caused increased paradoxical and asynchronous movements of the rib cage. The amount of asynchrony was not correlated with disease severity. Gosselink et al.19 reported increased VO2 and work of breathing in people with severe chronic obstructive pulmonary disease who performed diaphragmatic breathing with no spontaneous changes in respiratory frequency.
Dechman G20 reported that diaphragmatic breathing improves the ventilation, decreases work of breathing, decreases dyspnea and normalize breathing pattern in patients with chronic obstructive pulmonary disease.
Breathing techniques are included in the rehabilitation program of patients with chronic pulmonary disease (COPD). In patients with chronic obstructive pulmonary disease, breathing techniques aim to relieve symptoms and ameliorate adverse physiological effects by increasing strength and endurance of the respiratory muscles, optimizing the pattern of thoracic abdominal motion; and reducing dynamic hyperinflation of the rib cage and improving the gas exchange. Evidence exists to support the effectiveness
5
of purse-lip breathing, forward leaning position, active expiration and inspiratory muscle training but not for diaphragmatic breathing.
Breslin21 reported that, during pursed lip breathing there is a decreased diaphragm activity during inspiration and was accompanied by increased use of rib cage muscles. Both abdominal and rib cage accessory muscle activity increased during expiration. Respiratory rate decreased as did the duty cycle. In addition, Breslin’s21 estimate of the resting diaphragm tension-time index indicates that, as a group, the subjects were above the diaphragm fatigue threshold described by Bellemare and Grassino22 and this supports the outcome of Group A.
O’Donnell23 and colleagues proposed that people with chronic obstructive pulmonary disease have “a very fine control of expiratory flow whereby intra thoracic pressure is continuously adjusted to a level that is just enough to attain maximal flow”. Furthermore, they proposed that this active control develops with the disease process, suggesting that imposing retraining techniques is not uniformly helpful in this population and this supports the outcome of study.
Conclusion: This study can be concluded by stating that Pursed Lip Breathing is effective for alleviating the symptoms like dyspnea and airflow limitations; and both exercises are effective in improving the exercise tolerance in the management of chronic obstructive pulmonary diseases. This was shown by improvement inFEV1, FVC and six-minute walk test.
Keywords: Diaphragmatic breathing exercise, pursed lip breathing, stable chronic obstructive pulmonary disease, FEV1, FVC and six-minute walk test.
References:
1. www. GOLD COPD.com.
2. Susan b O’Sullivan Thomas schmite physical rehabilitation Assessment and Treatment 4th edition India: Jayapee brothers 2001 pp: 448.
3. Global initiative for chronic obstructive pulmonary disease (2006). 4. Anthony S. Fauci., Harrison’s principles of internal medicine, 14th edition, vol.2, USA: Mc Graw-Hill companies Inc.., 1998, pp, 1041-1046.
5. Belman et. Al., “Reliability of Borg scale for dyspnoea”. Chest Journal, 4, 2002, pp.37.
6. Dechman G., Wilson C.R., “Evidence underlying breathing retraining in people with stable COPD”, physical therapy, 84, 2004, pp.1189-1197.
7. Thoman: Comparison of the oxygen cost of breathing exercises and spontaneous breathing in patients with stable chronic obstructive pulmonary disease. Chronic Respiratory Disease July 2004 1:163-172.
8. Mueller RE, Petty TL, Filley GF. Ventilation and arterial blood gas changes induced by pursed lips breathing. J Appl Physiol 1970; 28, 784-789.
9. Killian KJ, LeBlanc P, Martin DH, Summers E, Jones NL, Campbell EJ. Exercise capacity and ventilatory, circulatory and symptoms limitation in patients with chronic air flow obstruction. Am. Rev. Respir. Disord. 1992; 46: 935-40.
10.Schans CPVD et al. Effects of positive expiratory pressure breathing during exercise in patient with COPD. Chest. 1994;105: 782-89.
11.Gosselink, R.” breathing technique in patients with chronic obstructive pulmonary disease (COPD)” chronic Respir dis.2004; 1(3):163-72 (issn:1479 -9723).
6
12.Jones AY1, Dean E, Chow CC : Comparison of the oxygen cost of breathing exercises and spontaneous breathing in patients with stable chronic obstructive pulmonary disease. Phys Ther. 2003 May;83(5):424-31.
13.Levensen CR: Breathing exercises in Zaidal, CC (ed) pulmonary Management in physical Therapy. Churchill Livingstone, New York,1992.
14.Vitacca, M.clini, E. Blanchi, LAmbrosino, N>” Acute effects of deep diaphragmatic breathing in COPD patients with chronic respiratory insufficiency “. European Respiratory journal,11,1998, pp.408-415.
15.Killian KJ, LeBlanc P, Martin DH, Summers E, Jones NL, Campbell EJ. Exercise capacity and ventilatory, circulatory and symptoms limitation in patients with chronic air flow obstruction. Am. Rev. Respir. Disord. 1992; 146: 935-40.
16.Brach BB, Chao RP, Sgroi VL, et al. 133Xenon washout patterns during diaphragmatic breathing: studies in normal subjects and patients with chronic obstructive pulmonary disease. Chest.1977 ;71:735–739.
17.Sackner MA, Gonzalez HF, Jenouri G, Rodriguez M. Effects of abdominal and thoracic breathing on breathing pattern components in normal subjects and in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis.1984; 130:584–587.
18.Tony Reybrouck, Clinical usefulness and limitation of 6 min walk test in patients with cardiovascular and pulmonary disease. Chest 2003; vol 23, no.2, pp 325-327. 19.Tony Reybrouck, Clinical usefulness and limitation of 6 min walk test in patients
with cardiovascular and pulmonary disease. Chest 2003; vol 23, no.2, pp 325-327. 20.Dechman G., Wilson C.R., “Evidence underlying breathing retraining in people with stable COPD”, physical therapy, 84, 2004, pp.1189-1197.
21.Breslin, EH. The pattern of respiratory muscle recruitment during pursed-lips breathing COPD. Chest 1992;101, 75-78.
22.Bellemare F, Grassino A. Effect of pressure and timing of contraction on human diaphragm fatigue. J Appl Physiol.1982; 53:1190–1195.
23.O’Donnell DE, Sanii R, Anthonisen NR, Younes M. Expiratory resistive loading in patients with severe chronic air-flow limitation: an evaluation of ventilatory mechanics and compensatory responses. Am Rev Respir Dis.1987; 136:102–107.
24.Levine S, Nguyen T, Friscia M, Zhu J, Szeto W, Tikunov BA, Kucharczuk JC, Rubinstein NA, Kaiser LR, and Shrager J. Parasternal intercostal muscle remodeling in severe chronic obstructive pulmonary disease. J Appl Physiol 101: 1297–1302, 2005.